Covid19 Guideline & Resources
COMMUNICATION HUB
A Comprehensive Repository of Risk Communication and Community Engagement (RCCE) materials
Here you can find a comprehensive collection of RCCE material for management of COVID-19 and the vaccination drive. These include RCCE materials issued by the Government of India, State Governments, UN, WHO, CDC and other national and international authorities. These can be used by health professionals, communities and people at large. The user can now search these by category, language, issuing organization or a combination of any of these filters.
 COMMUNICATION HUB
COMMUNICATION HUB
Healthcare Norms
Health institutions and health workers are on the front lines of the fight against COVID-19. Our efforts to curtail the spread of the virus hinge on the adaptability and commitment of our health workers and institutions. At the same time, they need protection from infection and form the stigma and discrimination that comes from the fear of the virus. This section contains health-care communication materials developed and used by USAID partners as well as other government and non-government agencies that empower health professionals and institutions to address this emergency as well as to help them get the respect and support they deserve.

 COMMUNICATION HUB
COMMUNICATION HUB
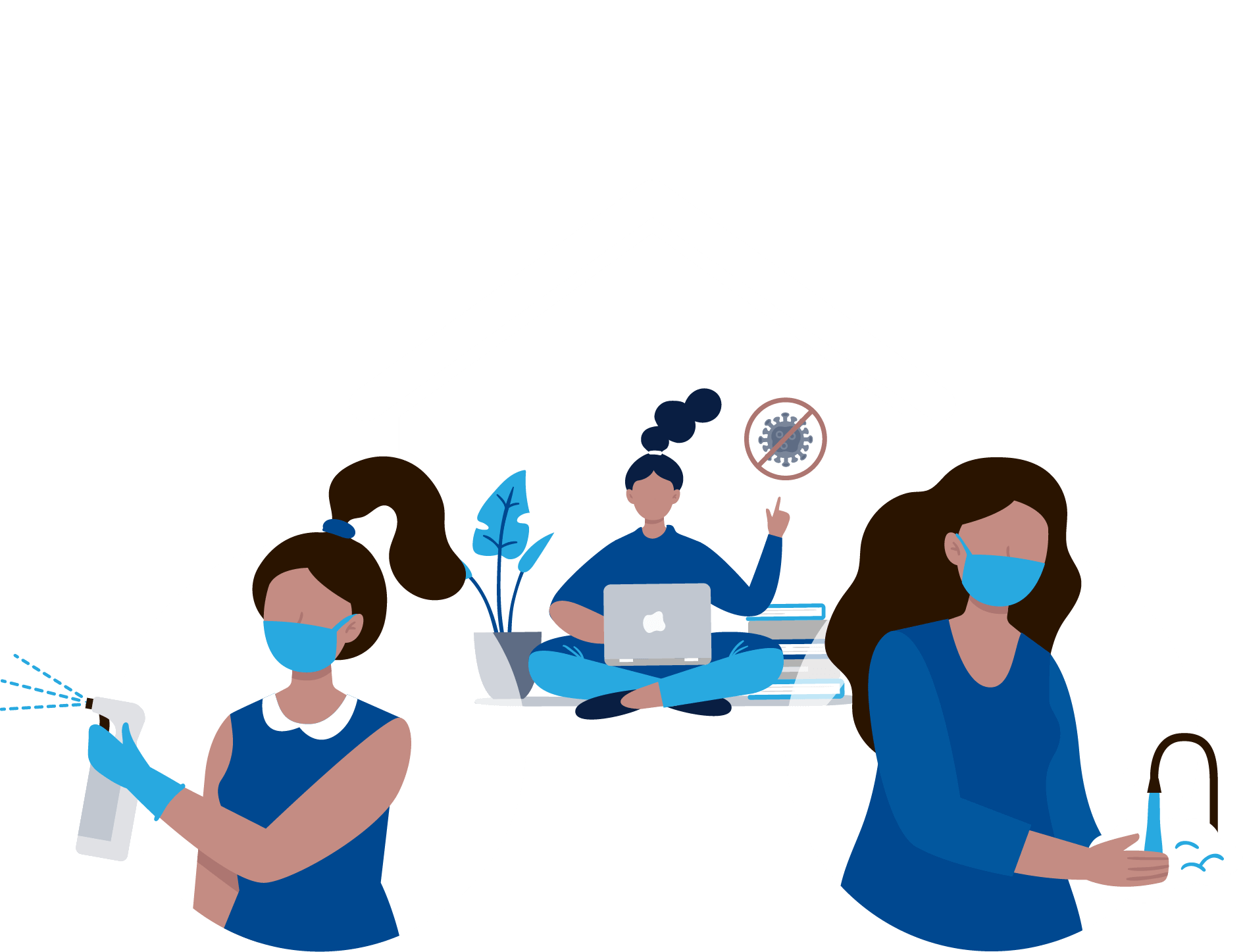
Self care
Here you can find a comprehensive repository of Risk Communication and Community Engagement (RCCE) materials developed and used by implementing partners supported by USAID/India and by other trusted sources across the health sector.
 COMMUNICATION HUB
COMMUNICATION HUB
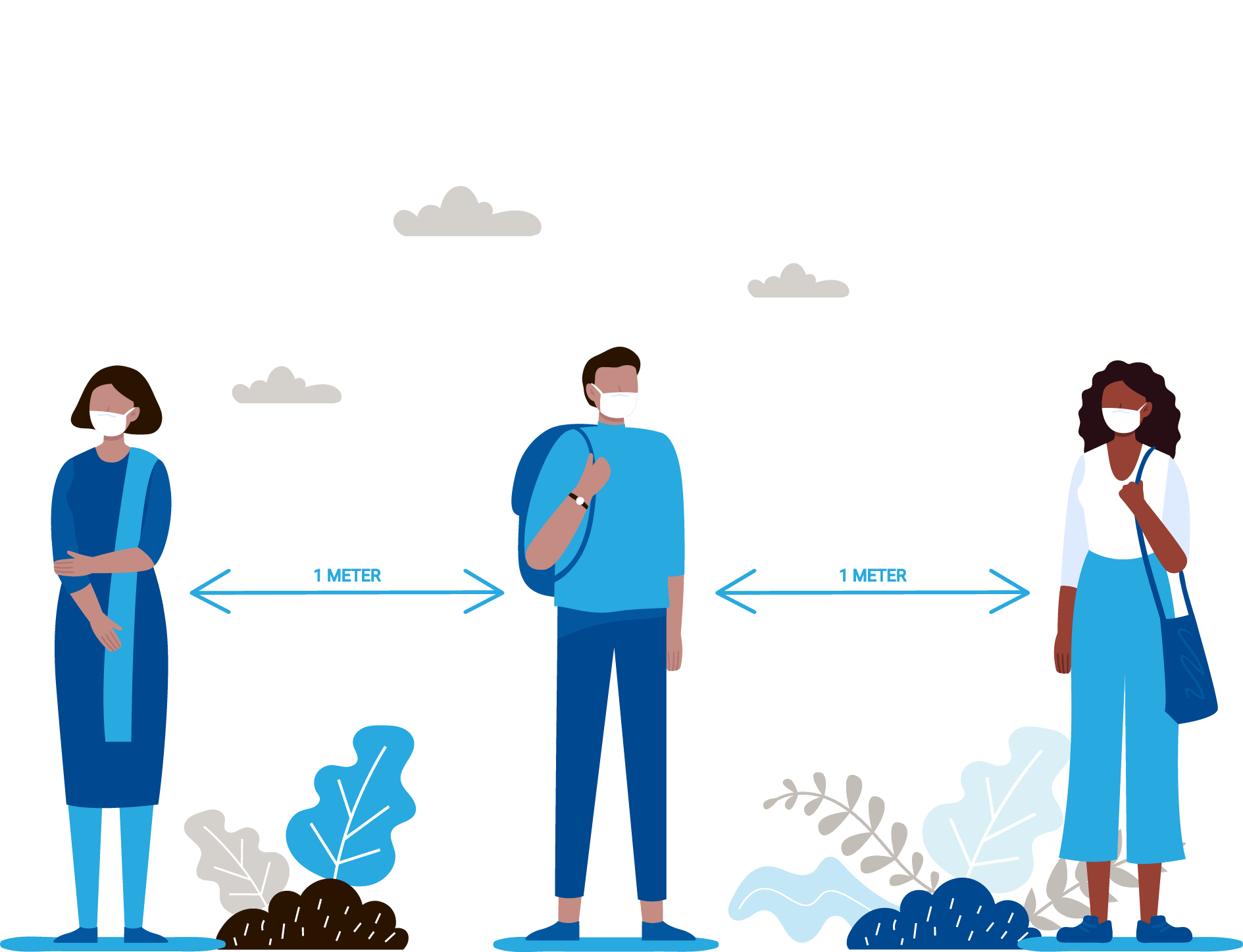
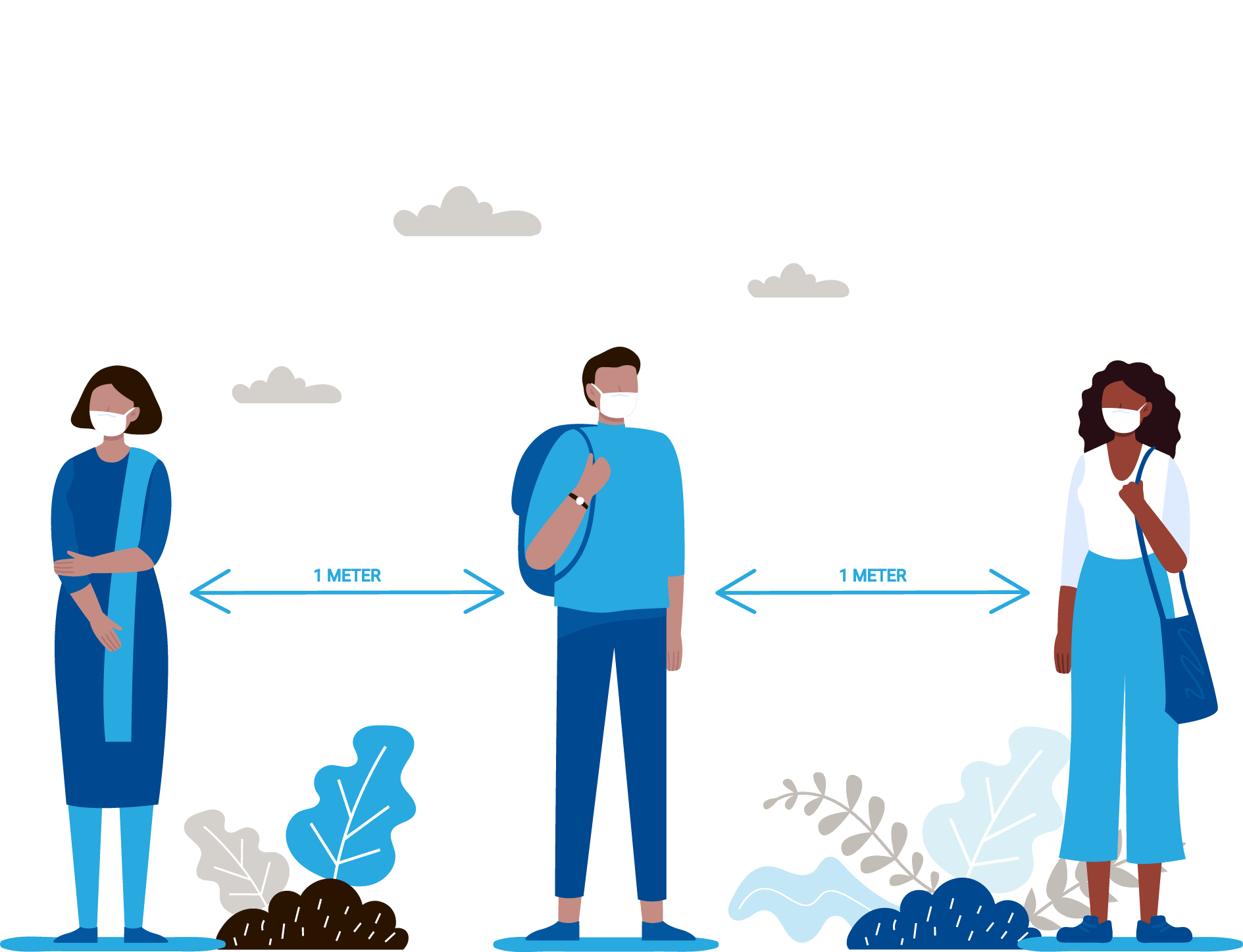
Social Norms
Community spread of COVID-19 has been one of the biggest challenges in the fight against the virus. It has created an urgent need for shifts in the behaviours and norms related to social interaction and community engagement. This page contains interpersonal communication materials developed and used by USAID partners as well as materials created by government and non-government agencies to empower communities to protect themselves and respond to those affected with respect and compassion.